Cardiovascular System disorders
Summary of drug discovery and development activities
During the reporting period several compounds were synthesised and evaluated for cardiovascular activities in cell culture and in animal models. Around 87, 73, 80, 80, 216 compounds were submitted for Anti-Inflammatory, Anti-hyperlipidemic, Anti-Angiogenic, Anti-NAFLD and Anti-adipogenesis activities, respectively. 12, 8 and 2 interesting hits were obtained in the anti-hyperlipidemia, anti-angiogenic and anti-adipogenic screens respectively which are being further validated in the respective laboratories. Furthermore, about 600 NCEs and natural products were submitted for GPCR profiling during last one year and several preliminary hits were identified that are being consolidated. Besides these, several standardized extracts like CDR267F018 were evaluated for cardiovascular activities under CSIR’s Phytomission.
New initiatives in the areas of CVS disorders
Several new dimensions were added to the area of cardiovascular research with the joining of new faculty in the Pharmacology department. A new area for the identification of novel theranostic targets in heart diseases was initiated. Cardiovascular diseases are the leading cause of mortality in India as well as globally. According to the recent data from Global Burden of Diseases, in India, cardiovascular diseases contributed to more than twenty-six percent of deaths in 2017. Heart failure characterized by inability of the heart to pump enough blood to the body, is the end-result of various pathological events collectively termed as cardiac remodelling. Morphologically, cardiac remodelling involves cardiomyocyte hypertrophy/atrophy, apoptosis, deregulated autophagy and interstitial fibrosis. Therefore, it is hypothesized that better understanding of cardiac remodelling process will help in identification of novel theranostic target, which might reduce cardiovascular disease burden. New studies are initiated on the exploration of novel RNA-binding proteins and circular RNAs as theranostic target. Workers aim to utilize viral gene therapy approach like adeno-associated virus to inhibit and increase the expression of these genes in diseased heart.

Augmentation of iNOS expression in myeloid progenitor cells expedites neutrophil differentiation
Neutrophils play an important role in immunity and inflammation through diverse mechanisms. Previously involvement of NO in neutrophil adhesion, chemotaxis, bacterial killing, reactive oxygen species generation, neutrophil extracellular traps' formation, and apoptosis has been demonstrated. Constitutive expression of iNOS in human neutrophils has also been documented. The role of NO-iNOS in neutrophil differentiation however remains ill-defined. Herein, studied the role of NO generated from iNOS in the neutrophil differentiation by using iNOS-overexpressing K562 cells (K562iNOS) and iNOS-deficient murine progenitor cells (lineage negative cells; lin-ve). It was observed that iNOS overexpression led to increased neutrophilic differentiation in K562 cells; more specifically an early and accelerated neutrophilic differentiation was spotted in K562iNOS. These observations were further validated using iNOS knockout lin-ve cells or hematopoietic progenitor cells that exhibited delayed neutrophil differentiation in comparison to its wild-type counterpart. In addition, a significant increase in the gene expression of iNOS during neutrophilic differentiation of CD34+ hematopoietic stem and progenitor cells derived from human bone marrow further substantiates importance of iNOS in neutrophil differentiation. Moreover, a significant increase in NO generation during neutrophil differentiation was observed and enhanced neutrophil differentiation with NO donor was also observed, implying the importance of NO in neutrophil differentiation. Collectively, using alternative approaches, it is demonstrated that neutrophil differentiation is significantly influenced by iNOS or NO, suggesting the possibility of exploiting this novel link for therapeutic aspects of NO generated from iNOS and neutrophil differentiation in hematopoiesis-related disorders. (J Leukoc Biol. 2019; 106(2): 397-412).
Role of P47phox in Angiotensin II induced cardiac hypertrophy and fibrosis in mice
NADPH oxidase mediated ROS production has been recognized to be an important contributory mechanism for hypertension and left ventricular hypertrophy (LVH). However, the regulatory role of NADPH oxidase mediated superoxide production in Angiotensin II (AngII) induced cardiac fibrosis and macrophage infiltration is still elusive. Herein, investigated the role of phagocytic NADPH oxidase enzyme system in cardiac remodelling induced by AngII in young adult (2-3 months old) male mice deficient in p47phox, a cytosolic subunit of the NADPH oxidase (KO, n=13) and age-matched wild-type littermates (WT, n=9). Animals were infused with AngII pressor dose (1500 ng/kg/min, s.c) or saline via osmotic mini pump for 14 consecutive days and subjected to echocardiography on the last day. Further animals were sacrificed and hearts were harvested for histological studies and gene expression analysis. AngII treatment in WT and KO mice showed prominent alterations in echocardiographic measurements with no changes in E/A, EF and FS. However, KO mice showed aggravated cardiac hypertrophic response (LVAWd: WT, 1.20±0.09 vs. KO, 1.42±0.04, p<0.05; LVIDd: WT, 3.02±0.20 vs. KO, 2.60±0.07, p<0.05; LVPWd: WT, 1.49±0.06 vs. KO, 1.78±0.06, p<0.05). Histologically, AngII infused KO mice also showed increased cardiomyocyte diameter compared to AngII infused WT mice (WT, 388±16.37 vs. KO, 560.3±41.28 μm2; p<0.01 respectively). Further, AngII infused KO mice showed elevated immune cell infiltration, which were positive for Mac-3 staining compared to AngII infused WT mice (WT, 2.61±0.32 vs. KO, 4.09±0.44 %; p<0.05). Besides, AngII infused KO mice showed augmented interstitial fibrosis (WT, 11.11±0 0.67 vs. KO, 20.85± 3.63 %; p<0.05), thick collagen fibres deposition (WT, 28.93± 0.94 vs. KO, 37.60± 2.49 %; p<0.05) compared to AngII infused WT mice. Moreover, AngII infused KO mice also showed upregulated gene expression of hypertrophic and fibrotic markers, including Nppa, Nppb, Acta1, Myh6, TGF-β1, collagen (I and III) and α-sma compared to AngII infused WT mice. Together, these data suggest that NADPH oxidase and its subunit p47phox play a pivotal role in AngII induced LVH by regulating fibrotic machinery and macrophage infiltration (Hypertension, 2019; Vol. 74, No. Suppl-1).
Temporal immmunometabolic profiling of adipose tissue in HFD-induced obesity: Manifestations of mast cells in fibrosis and senescence
Chronic low-grade inflammation/meta-inflammation in adipose tissue leads to obesity-associated metabolic complications. Despite growing understanding, the roles of immune cell subsets, their interrelationship and chronological events leading to progression of obesity-associated insulin resistance (IR) remains unclear. Herein, carried out temporal immunometabolic profiling of adipose tissue from C57BL/6 mice fed a high-fat diet (HFD) for 4, 8, 12, 16, and 20 weeks. Clodronate sodium liposomes (CLODs) were used to deplete macrophages and disodium cromoglycate sodium liposomes (DSCGs) to stabilize mast cells. In the temporal HFD settings, mice showed progressive glucose intolerance, insulin resistance, and adipose tissue senescence. Histochemical analysis of epididymal white adipose tissue (eWAT) using picro-sirius red and Masson's trichrome staining showed extensive collagen deposition in the 16th and 20th weeks. Flow cytometry analysis of the stromal vascular fraction (SVF) from eWAT revealed T-cell subsets as early-phase components and pro-inflammatory macrophages, as well as mast cells as the later phase components during obesity progression. In this therapeutic strategy, macrophage depletion by CLOD and mast stabilization by DSCG attenuated obesity, adipose tissue fibrosis, and improved whole-body glucose homeostasis. In addition, mast cell stabilization also attenuated senescence (p53 and X-gal staining) in eWAT, signifying the role of mast cells over macrophages during obesity. The study emphasizes on the new-generation mast cell stabilizers that can be exploited for the treatment of obesity-associated metabolic complications (Int J Obes (Lond). 2019; 43(6): 1281-1294).
Pro-inflammatory effect of EMP is dysfunctional mitochondria mediated and modulated through MAPKAPK2 leading to attenuation of cardiac hypertrophy
This Study showed the functional significance of mitochondria present in EMP and how MK2 (MAPKAPK2) governs EMP production and its physiological effect on cardiac hypertrophy. Flow cytometric analysis, confocal imaging, OCR measurement through Seahorse were used to confirm the presence of functionally active mitochondria in non-treated EMP (c-EMP), LPS and oligomycin treatment increased mitochondrial ROS activity in EMP (l- and o-EMP, respectively). The dysfunctional mitochondria contained in l- and o-EMP induced the expression of pro-inflammatory mediators in the target endothelial cells leading to the augmented adhesion of THP-1 monocyte cells on EA.hy926 cells. Multiphoton real-time imaging detected the increased adherence of o-EMP at the site of carotid artery injury as compared to c-EMP. MK2-deficient EMP reduced the E-selectin and ICAM-1 expression on target endothelial cells leading to reduced monocyte attachment and reduced cardiac hypertrophy in mice. In conclusion MK2 promotes the pro-inflammatory effect of EMP mediated through dysfunctional mitochondria. MK2 modulates the inflammatory effect induced during cardiac hypertrophy through EMP. (Arterioscler Thromb Vasc Biol. 2019 Jun; 39(6): 1100-1112).
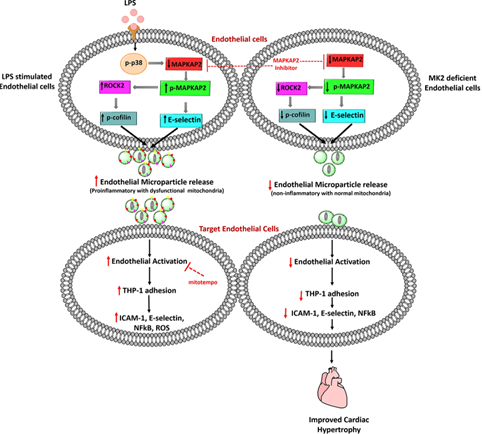
Fig 01: Cartoon depicting how dysfunctional mitochondria loaded EMP regulates pro-inflammatory mediators via MAPKAPK2
Involvement of fatty acid synthase in right ventricle dysfunction in pulmonary hypertension
Apart from pulmonary vascular resistance and right ventricle (RV) hypertrophy, metabolic dysfunction also plays a major role in pathophysiology of pulmonary hypertension (PH). Recently, it was shown that fatty acid synthase (FAS), an enzyme involved in de novo fatty acid synthesis, plays a pivotal role in PH as its inhibition was protective and decreased pulmonary vascular remodelling, RV pressure and hypertrophy and improved endothelial functions. However, the precise mechanism behind protective effect of FAS inhibition on right ventricle dysfunction associated with PH is not completely understood. In this study, delineated the mechanism of protective effect of FAS inhibition on RV dysfunction associated with PH. siRNA mediated inhibition of FAS reduced FAS expression, hypertrophy, inflammation, apoptosis, autophagy and improved the glucose oxidation, mitochondrial membrane potential and ATP level in hypoxic cardiomyocytes. In monocrotaline (MCT) treated rats, FAS inhibition by C75 (2 mg/kg, i.p., once a week from 21 to 35 days) decreased the expression and activity of FAS and palmitate level. C75 also improved cardiac functions and mitochondrial membrane potential leading to decreased apoptosis in RV of MCT treated rats. In conclusion, this study reveals that inhibition of FAS decreases RV hypertrophy and improves cardiac function associated with PH by perking up metabolic functions. (Experimental Cell Research 2019; 383 (2); 111569)
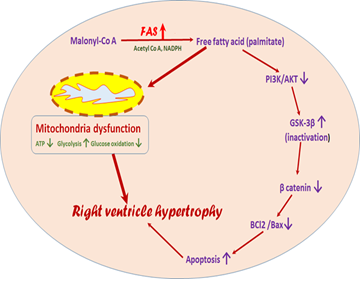
Fig 02: Cartoon depicting how Fatty Acid Synthase alters metabolism and regulates right ventricle hypertrophy associated with pulmonary hypertension
Multifactorial functions of the inflammasome component NLRP3 in pathogenesis of chronic kidney diseases
The NLRP3 inflammasome plays a central role in necroinflammation by sensing danger signals and releasing proinflammatory cytokines and regulating pyroptosis. Inflammasome activation mainly in the renal mononuclear phagocytes but also in the renal parenchymal cells results in the release of proinflammatory cytokines, IL-1b and IL-18, which sets up renal inflammation during chronic kidney disease (CKD). Therefore, propose the inflammasome–IL-1/IL-18 axis as a promising therapeutic target for CKD. In addition, recent data emphasize the inflammasome-independent roles of NLRP3 in nonimmune cells of the kidney. Especially, the inflammasome-independent proapoptotic and profibrotic functions of NLRP3 and ASC contribute to kidney disease pathogenesis. Thus, also propose NLRP3 and ASC as putative targets to combat renal fibrosis during CKD progression, especially given the multifactorial functions of NLRP3. The kidney comprises a variety of cells, each with specified functions. However, functions of the NLRP3 inflammasome and its components in individual renal cells and their contribution to CKD remain to be explored. Therefore, studies using cell type – specific inflammasome related protein knockout mice for CKD animal models are needed in the future. (Kidney Int. 2019; 96(1): 58-66.)
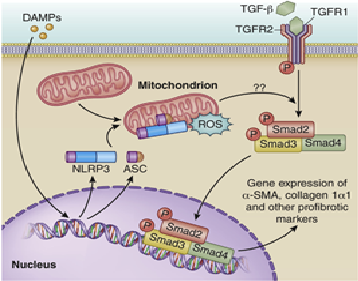
Fig 03:Inflammasome-independent NLRP3-mediated renal fibrosis.
Mitochondrial dynamics and immune regulation during inflammatory disorders
Crohn’s disease (CD) and ulcerative colitis (UC), the main clinical pathologies of inflammatory bowel disease (IBD), arise due to the inter-play of genes that regulate immune function. In the susceptible host, an altered gut flora leads to an unbalanced cytokine production and tight junction dysfunction resulting in chronic inflammation and pain in the intestine. Mitochondria have recently emerged as an important organelle that regulates antibacterial and antiviral immune pathways and these functions are intimately linked to their morphology. Cellular mitochondria constantly undergo fusion, fission, directed movement in the cell and mitophagy mediated clearance-collectively termed as 'mitochondrial dynamics'. Studies have demonstrated decreased mitochondrial electron transport chain complexes in the IBD patients and a dysregulated release of mitochondrially-derived reactive oxygen species (MT-ROS) suggesting dysfunctional mitochondria. There are multiple proteins that coordinate to regulate the mitochondrial dynamics. This preliminary data indicate a strong role for mitochondrial dynamics components in regulating immune response and tampering with the mitochondrial localization altered the clinical outcome in the IBD animal model.
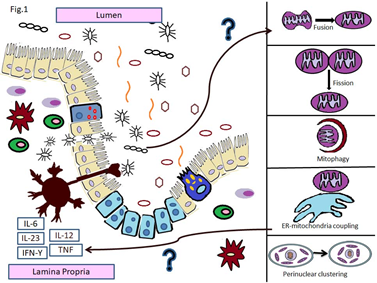
Fig 04:Role for mitochondrial dynamics in regulation of immune response in IBD.
Fructose-induced AGEs-RAGE signaling in skeletal muscle contributes to impairment of glucose homeostasis
Increased fructose intake has been linked to the development of dyslipidemia, obesity and impaired glucose tolerance. Due to its specific metabolic fate, fructose impairs normal lipid and carbohydrate metabolism and facilitates the non-enzymatic glycation reaction leading to enhanced accumulation of advanced glycation end products (AGEs). However, the formation of fructose-AGEs under in vivo setup and its tissue specific accumulation is less explored. Herein, investigated the impact of high fructose on AGEs accumulation in skeletal muscle and its causal role in impaired glucose homeostasis. In L6 rat skeletal muscle cells, chronic exposure to fructose induced AGEs accumulation and the cellular level of the receptor for AGEs (RAGE) and the effect was prevented by pharmacological inhibition of glycation. Under in vivo settings, Sprague Dawley rats exposed to 20% fructose in drinking water for 16 weeks, displayed increased fasting glycemia, impaired glucose tolerance, decreased skeletal muscle Akt (Ser-473) phosphorylation, and enhanced triglyceride levels in serum, liver and gastrocnemius muscle. It was also observed a high level of AGEs in serum and gastrocnemius muscle of fructose-supplemented animals, associated with methylglyoxal accumulation and up regulated expression of RAGE in gastrocnemius muscle. Treatment with aminoguanidine inhibited fructose-induced AGEs accumulation and normalized the expression of RAGE and Dolichyl-Diphosphooligosaccharide-Protein Glycosyltransferase (DDOST) in gastrocnemius muscle. Inhibition of AGEs-RAGE axis counteracted fructose-mediated glucose intolerance without affecting energy metabolism. These data reveal diet-derived AGEs accumulation in skeletal muscle and the implication of tissue specific AGEs in metabolic derangement, that may opens new perspectives in pathogenic mechanisms and management of metabolic diseases. (The Journal of Nutritional Biochemistry (2019); 71:35-44).